Tips for How to Manage Medical Specialty Triage Calls
How to Manage Medical Specialty Triage Calls (PDF)
Many call center leaders and triage nurses report the complexity of triage calls has increased in recent years. One factor that has been attributed to this increased complexity is the increasing number of patients with chronic illnesses. A related factor identified is the management of specialty practice calls. In the Schmitt-Thompson Clinical Content (STCC) Nurse Triage Contact Center Benchmarking Survey (2023), about a third of call centers reported taking specialty calls (33% during afterhours; 28% during daytime hours).
It is important to note that the principles and components of telehealth nurse triage remain the same across all patient populations. Regardless of practice setting, the triage nurse must conduct a focused, organized assessment, select an appropriate triage guideline(s), and refer the patient to a safe, appropriate level of care.
For the purpose of this newsletter, we define specialty triage as symptom-based triage of a designated group of patients that have an illness that has specialty care oversight. The triager could be representing and triaging on behalf of a specialty clinic, or triaging a primary care patient that also sees a specialist or has an illness that qualifies for specialized care. A specialty clinic supports patients as part of a designated group, disease process or treatment. Examples are urology, gastroenterology or neurology.
In the pages that follow we outline some tips on how to approach medical specialty-related calls. We also discuss some steps a call center can take to help ensure success before formally taking on calls from a new medical specialty practice.
Why Is Specialty Triage a Concern for All Nurse Triagers?
Patients with complex medical problems often see a number of specialists in addition to their primary care provider. A call center nurse may receive a call from a patient regarding a specialty practice problem, regardless of whether or not that call center takes calls for that specialty practice. It is likely that you may already be receiving such calls.
Likewise, a nurse triaging within a specialty office during office hours may receive a call from a patient who presents with a non-specialty problem. For example, a triage nurse who takes calls in an OB clinic during office hours may receive a call from a pregnant patient who reports sudden shortness of breath and positive COVID test.
At a minimum, the triage nurse in both cases needs to rule out life-threatening symptoms before referring the patient to an appropriate on-call provider or other designated resource.
Where to Start – Focus on the Reason for Call (Primary Chief Complaint)
Best practice for telehealth triage nursing is to identify the primary reason for call (chief complaint) and to triage the symptom(s).
For most specialty practices, the majority of calls are symptom-related.
Even for specialty calls, focusing on the primary reason for call (symptoms such as abdomen pain, cough, chest pain) is usually the best place to start.
Next, it is important to determine if this symptom is a new problem. If the answer is No, ask: Is the symptom the same, worse, or better than the patient’s normal (baseline).
Ask About Recent and Chronic Medical History
An important part of the initial assessment is asking the patient about recent medical history (recent hospitalizations or procedures, injuries, medical visits, new medicines).
The triager should then be prompted to consider and investigate further to determine if a recent or chronic illness may be contributing or related to the caller's current chief complaint.
The initial assessment questions can help guide the triager in this assessment.
Which Guideline(s) Should I Use?
Occasionally we get these questions from customers:
Are the STCC guidelines written specifically for primary care triage?
Can we use the general symptom-based guidelines for specialty triage?
The STCC guidelines have been written to ensure clinical safety and consistency of responses to symptom-based questions. The focus of triage, whether it be on behalf of primary or specialty care patients, is to triage the patient by symptom.
Within a symptom-based guideline, important risk factors related to chronic illness or medical care are addressed in triage assessment questions (TAQs). See examples in table below:
There are also triage questions that address chronic symptoms, which are often managed in a specialty practice. See examples below:
Finally, in each guideline there are SMAGs (See More Appropriate Guideline statements) that direct the triager to a more specific guideline that is best to use. In some cases, the SMAG is for a “specialty” guideline available in the STCC adult guideline set. See examples in table below. It is important to review and pay close attention to the SMAGs in each guideline.
Now more than ever, it is important for the triage nurse to be aware of the types of triage guidelines available. Currently there are 417 adult guidelines, with new guidelines added every year.
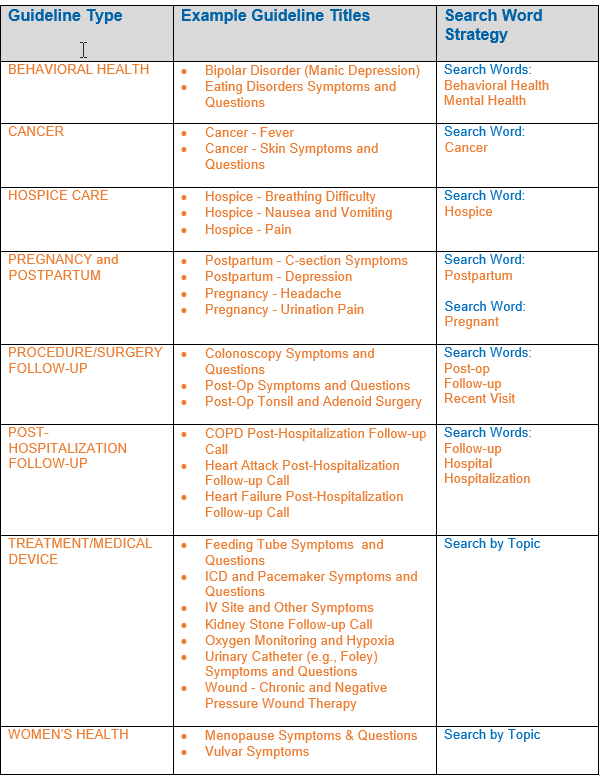
Below, we outline some of the types of specialty guidelines available and Search Word strategies to help the nurse efficiently search for and select the most appropriate guidelines.
Clinical Judgment Is Key
The triage nurse must always use clinical judgment with every call. This is even more important when the patient has one or more chronic diseases and comorbidities.
When responding to a call from a specialty practice, the triager may encounter a problem or concern not addressed in the guideline. The triager may use an additional approved resource if one is available to answer the caller’s question. If none is available, the triager will need to use clinical judgment in these situations. One option is consultation with the provider on-call.
There are TAQs within many of the guidelines to help the triager document their response to these calls:
Caller has urgent question AND [2] triager unable to answer question
Caller has non-urgent question AND [2] triager unable to answer question
Sometimes the triager may feel, based on clinical judgment, the guideline recommended disposition is less or more urgent than might be warranted for a given patient situation. Again, it may be best in those situations to consult with the provider or have the provider triage the patient (secondary triage).
Strategies to Consider Before Formally Taking Calls From New Specialty Practice
Review the existing STCC guidelines and identify gaps:
We recognize there will likely be some situations not covered in the current STCC triage guidelines.
We also recognize local care practices may differ from what is outlined in guideline care advice (e.g., post-op). Health care practice standards and health care resources can vary by location. Review the current guidelines to determine if there are any gaps.
Customize guidelines:
Local call centers have permission to make modifications to the Schmitt-Thompson Clinical Content (STCC) to reflect local healthcare practices and resources. For example, a disposition level can be customized with approved medical oversight (i.e., specialty liaison). Note: This can be time-consuming to manage with the guidelines being updated yearly.
Add additional resources:
Offer additional reference material for the triager to use in addition to the guideline dispositions and care advice. This could include a treatment protocol, discharge materials, pre-procedure instructions or standing orders.
This can be imbedded in the software or easily accessed by the triager as a health education topic, a predefined phrase or “dot or smart phrase.” Check with your software vendor on available options.
Educate and prepare staff:
Preparing triagers with education and resources can help increase comfort and proficiency with specialty triage knowledge. Here are some areas of focus:
Collect data: Identify the top 5 to 10 calls that the specialty clinic takes. Work with the specialty clinic liaison to review these symptoms or procedures. Make available appropriate resources or references to the triagers.
Review specialty practice patient resources: Review available patient-specific information for the specialty clinic (e.g., pre- or post- procedure, treatment care plans, discharge instructions). Share with staff. Imbed in software if possible.
Develop 2nd level triage process: What steps should the nurse triager take when uncertain of best advice or there is another reason for provider consultation? Outline this process in a policy.
Determine scope: Will all nurses be trained to the specialty calls, or only designated triagers?
Orient staff: Role play triage calls based on top 10 specialty calls. Allow for questions and discussion. Share findings and questions with staff. Outline documentation standards.
Identify key resources from specialty practice: Are there specialty nurse triagers or providers that can help train, orient or do call review?
Provide ongoing education: Consider case studies, periodic in-services, and ongoing feedback based on call and chart review as well as specialty provider feedback.
Co-Authors:
Jeanine Feirer, RN, MSN, Nurse Editor, Adult Clinical Content
Cheryl Patterson, RNC-TNP, BSN, Nurse Editor, Adult Clinical Content
References
Ansah JP, Chiu CT. Projecting the chronic disease burden among the adult population in the United States using a multi-state population model. Front Public Health. 2023; 10:1082183. Published 2023 Jan 13.
Boersma P, Black LI, Ward BW. Prevalence of Multiple Chronic Conditions Among US Adults, 2018. Prev Chronic Dis. 2020;17: E106. Published 2020 Sep 17.
Rutenberg, C., & Greenberg, M.E. (2012). The art and science of telephone triage: How to practice nursing over the phone. Pitman, NJ. Anthony J. Janetti, Inc.