Tachypnea in Pediatrics: Triage Assessment Tips
With respiratory season fast approaching, call centers and offices prepare for call volume surges regarding respiratory viral infections. Tachypnea (increased respiratory rate or RR) is often the earliest sign of mild respiratory distress in children and can represent hypoxia. Young infants with any respiratory illness can rapidly develop distress and hypoxia. Respiratory failure is the most common pathway to a fatal outcome in children less than two years of age. This newsletter looks at some data and evidence regarding pediatric tachypnea. We also offer suggestions on how to efficiently triage this complaint while being conscious of call times.
Fever Does Not Cause Tachypnea
Fever is common in children with respiratory illness and up to 20% of children’s emergency department (ED) visits involve fever.1 Fever is the body’s normal response to infection. It can be due to self-limited mild illness or by more serious causes.
Some telehealth nurses may still assume that fever causes increased respiratory rates in children due to an increased metabolic rate. However, newer evidence and data contradict that and states that increased temperature does not have any impact on the respiratory rates or on oxygen saturation in children.
A study published in 2022 (Heal, et al) looked at over 235,000 pediatric patients presenting to emergency and urgent care and found there was no association between elevated temperature and changes in respiratory rate. In fact, for every 1⁰ C increase in temperature, there was an average 0.3% decrease in respiratory rate. So, in other words, no significant change. The study also found there was no clinical influence of temperature on oxygen saturation. However, they did find that for every 1⁰ C increase in temperature, heart rates increase on average 12 beats per minute (bpm). That is equivalent to about 7 bpm for every 1° F increase in body temperature.
ED Diagnoses in Children with Tachypnea
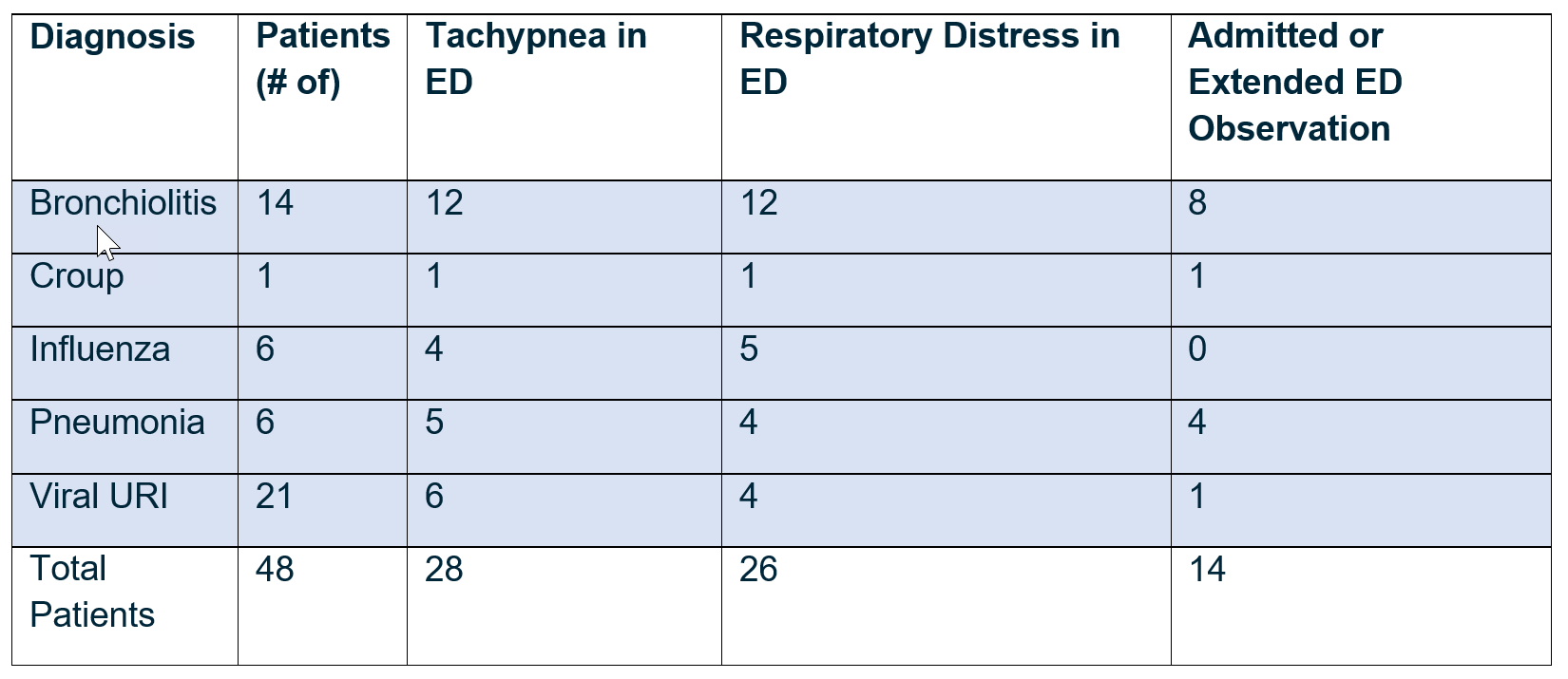
In an outcome data study done at Children’s Hospital Colorado Pediatric Call Center (Massaro, 2017), we looked at the diagnosis and ED course of 48 calls about children reported to be tachypneic sent in the ED. The study looked at the Cough guideline with this positive triage indicator: “Rapid breathing (Breaths/min > 60 if < 2 mo; > 50 if 2-12 mo; > 40 if 1-5 years; > 30 if 6-11 years; > 20 if > 12 years old)”. 28/48 (58%) of calls with telehealth nurse assessment as tachypneic also had documented tachypnea upon arrival to the ED. This study also did not show any consistent correlation between fever and tachypnea.
We did find that there were sick children sent in by this tachypneic triage indicator. Fourteen (29%) of the children were either admitted (13%) or had extended observation in the ED (16%). Three who were observed in the ED went home on oxygen. Here is a breakdown of their ED diagnoses
Triage Efficiency Tips: When Counting the RR is Not Needed
You do not need to count the RR in a child already confirmed by caller to have other signs of respiratory distress (e.g., retractions, nasal flaring, use of accessory muscles in older children, prolonged expiratory phase, cyanosis, belly breathing, etc.). Send these children in to the ED without counting the RR.
Counting the RR is also not needed if there are adventitious breath sounds present such as stridor, wheezing, or grunting per the caller. You only need to count the RR when the caller says the patient is “breathing fast” without any of the other higher triage questions being positive.
Triage Tips: How to Assess and Document RR When It is Needed
Although counting respiratory rate adds time to your calls, it is necessary if that is the chief complaint (or you need to do a full respiratory assessment). Follow these tips to try to ensure an accurate count:
Make sure the child is calm and still. Assess for 30 seconds and multiply by 2.
Listening to the child early on can help, although sometimes the nurse can’t hear the breathing well enough to count (especially with cell phones). If on a cell phone, request the caller to take off "speaker phone" to reduce echo and background noise or ask if they have a landline to improve communication quality.
If this assessment proves difficult, you could ask to receive a video clip or audio clip of the child’s breathing (depending on your software platforms accepting this media form). This often is more helpful and efficient than trying to hear the child over the phone.
If none of the above tips work, you will need to explain to the caller how to measure this.
Summary: Clinical Points for Triagers
Fever does not cause tachypnea nor increased work of breathing. Tachypnea is most often caused by lung disease (such as pneumonia or bronchiolitis) until proven otherwise. It's often the earliest sign of mild respiratory distress and can indicate hypoxia.
In infants, significant nasal congestion can lead to tachypnea which can be resolved by suctioning. Obligate nasal breathing can be a factor during the first 4 months of life. If the child is acting okay and feeding fairly well, consider calling these families back after nasal suctioning.
In the absence of respiratory symptoms, tachypnea can also be caused by metabolic acidosis, such as DKA, as the body tries to compensate.
Follow the triage efficiency points for guidance on when an objective measurement of the RR is needed.
Since fever causes tachycardia, expect the heart rate to decrease with fever reduction. If it doesn’t, there may be other factors to consider including dehydration, pain, or more serious illness (such as myocarditis).
Authors
Kelli Massaro, RN, Senior Nurse Editor, Pediatric Clinical Content
Bart Schmitt, MD, Medical Editor, Pediatric Clinical Content
Sam Wang, MD, Medical Editor, Pediatric Clinical Content
References
1. Heal C, Harvey A, Brown S, et al. The association between temperature, heart rate, and respiratory rate in children aged under 16 years attending urgent and emergency care settings. Eur J Emerg Med. 2022 Sep 6;29(6):413-416.
2. Massaro, K. Outcome data on tachypnea referred to the ED with the pediatric Cough guideline. Unpublished, 2017.
3. Schmitt B, Wang GS. Cough After Hours Pediatric Telehealth Triage Guideline. Schmitt Pediatric Guidelines, LLC. Copyright 2025.