Monkeypox (Mpox) Update for Telehealth Triage
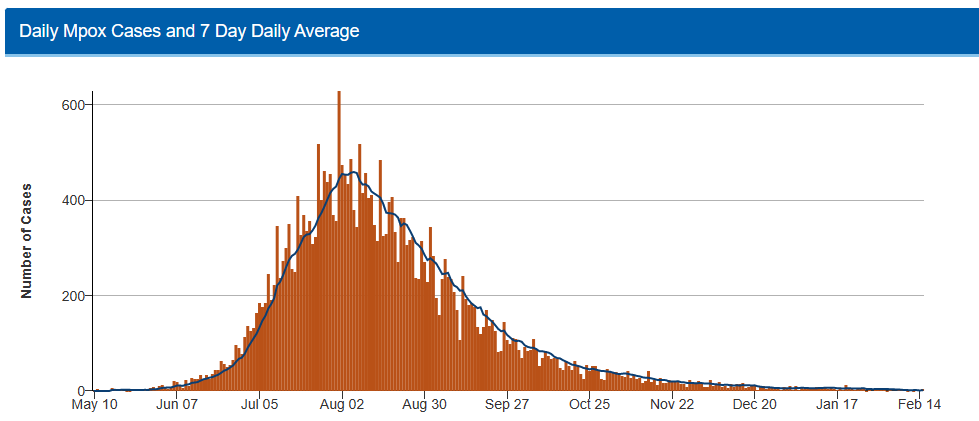
Monkeypox (Mpox) became a worldwide health concern in 2022. The first reported case in the United States was reported in May 2022. Both United States and Canadian cases of Mpox rapidly increased over the following months. To date there have been about 30,000 cases of Mpox in the United States and 1,500 cases in Canada.
As we move into 2023, reported case counts at the Centers for Disease Control and Prevention (CDC) show a substantial decrease.
However, Mpox continues to be a fairly common telehealth triage call.
In this newsletter, we summarize some important educational points about Mpox for telehealth triagers.
Triagers should strongly suspect Mpox if a person has symptoms of Mpox, such as an unexplained rash with fever, muscle aches, or swollen lymph nodes; and any of the following exposures in the past 21 days:
Skin-to-skin contact (e.g., hugging, kissing, massaging, having sex) with someone with Mpox.
Contact with materials (e.g., bed linens, clothing, sex toys) contaminated with Mpox.
Recent travel to a country where Mpox is endemic (e.g., Central and West Africa).
Not wearing a facemask during prolonged close contact (e.g., within 6 feet or 2 meters, for 3 hours or longer) with an unmasked person with Mpox.
General Information
Name
The World Health Organization (WHO) has renamed Monkeypox to Mpox. The disease was originally named when the virus was discovered in a group of captured monkeys (1958). The CDC is also switching from the term Monkeypox to Mpox.
We will be changing the titles of the two current adult telehealth triage guidelines to read Mpox instead of Monkeypox. These updated guidelines will be available in Spring 2023 with the annual update.
· Mpox - Diagnosed or Suspected
· Mpox - Exposure
How It Is Spread
Mpox can be spread from person-to-person. Most spread appears to occur from direct contact with infected sores, scabs, and body fluids. In North America, most spread occurs by direct skin contact during sex (anal, oral, vaginal). Mpox can also be spread by respiratory droplets between people with close face-to-face encounters. It can also be spread by touching objects that have infectious body fluids on them (e.g., bedding, towels).
Incubation Period
Symptoms usually start between 1 to 2 weeks after exposure. Range is from 4 to 21 days.
Symptoms
The most common symptom is rash (92%). Other symptoms are malaise (67%), fever, headache and itching (64%), chills, and enlarged lymph nodes.
Complications
Nearly all adults (99%) who get Mpox will survive. People can sometimes develop scars or pockmarks from the Mpox sores. Other complications are fairly rare.
Diagnosis and Testing
A doctor (or NP/PA) can suspect the diagnosis of Mpox based on a person's symptoms and confirm the diagnosis with testing (PCR test).
Special Populations at Risk
Nearly all of the current monkeypox cases occur in adult men. Most cases occur in men who have sex with men. Mpox should be suspected in men who have sex with men who also have typical symptoms of monkeypox.
However, anyone who has been in close contact with someone who has Mpox can get the illness.
Here are four special populations at risk for more severe illness.
Children 0 to 12 Years of Age
Notes:
Highest risk is infants less than 1 year of age.
Mpox cases in children had transmission from diagnosed caregivers, suspected through skin-to-skin contact and possibly a fomite. Limited data available.
No known secondary transmission from diagnosed child to other children (e.g., childcare facilities, school).
Triager Tips:
Reassure parents. Mpox is very rare in children.
Concerning rashes can be evaluated per guideline decision support.
Avoid known exposure to people that are suspected of having, or diagnosed with Mpox (e.g., skin-to-skin contact, respiratory droplet).
People with Weak Immune Systems or Chronic Skin Diseases (e.g., Eczema)
Notes:
Increased risk for severe disease.
Triager Tips:
Encourage safe sexual practices and avoid known exposure to people suspected of having Mpox.
If high risk sexual behavior, encourage the immunocompromised caller to talk with their doctor about pre-exposure vaccination.
Those with chronic skin diseases can talk with their doctor about vaccination.
Pregnant Women
Notes:
The Mpox virus can be transmitted in pregnancy to the fetus, and to a newborn via skin-to-skin contact.
There have been cases of spontaneous pregnancy loss, stillbirth, preterm delivery and newborn infections.
Rash in pregnancy AND known Mpox risk factors should have prompt evaluation.
Triager Tips:
Offer reassurance. Triage per decision support in guidelines.
The anti-viral medicine tecovirimat may be an option for a pregnant person. This medicine is not currently approved by the FDA for use with Mpox. Refer a pregnant person to their doctor (or NP/PA) for evaluation. Their doctor will work with the CDC to make the best plan for the patient.
Breastfeeding Women
Notes:
The physical and emotional importance of breastfeeding should be considered when triaging a mother with Mpox. Development of a thoughtful care plan with mother, doctor, lactation specialist and pediatrician input is imperative.
Due to the risk of a severe newborn infection, breastfeeding is not recommended if the mother has Mpox.
No skin-to-skin contact and separate rooms are recommended while the mother is infectious.
It is not known if the Mpox virus is in breast milk. CDC guidelines recommend that breast milk be discarded.
Triager Tips:
Reassurance and emotional support of the breastfeeding family is a priority.
Follow isolation care advice per Mpox guidelines.
If the mother chooses to hold the infant, follow CDC guidelines: gloves, gown and mask for mother, swaddling of infant, and no skin-to-skin contact.
Consider risk factors for postpartum depression if temporary isolation of the mother or alternative newborn feeding plans are in place.
Vaccination for Post-Exposure Prevention
There are two smallpox vaccines that can also be used for post-exposure (after an exposure) prevention of Mpox.
ACAM2000 Vaccine (U.S.): This is a live vaccine. It has more serious side effects than the MVA vaccine. It is not being used in the current outbreak.
MVA Vaccine (IMVAMUNE in Canada, JYNNEOS in U.S.): The most common side effects are itching, pain, redness, and swelling at the injection site. People may also have minor reactions such as feeling tired, headache, a mild fever, and muscle aches. Severe reactions (e.g., allergic reaction, anaphylaxis) are rare.
Vaccination works better the sooner it is given. Ideally, it should be given within 4 days of exposure. Vaccination can be considered for up to 14 days after an exposure according to the CDC.
STCC Telehealth Triage Guideline Resources
Adult
Mpox – Diagnosed or Suspected (Adult)
Mpox – Exposure (Adult)
Immunization Reactions (Adult)
Pediatric
Rash or Redness – Localized
Rash or Redness – Widespread
Penis-Scrotum Symptoms – After Puberty
Vaginal Symptoms or Discharge – After Puberty
STI Exposure or Questions
References and Resources
Canada.CA: Available at https://www.canada.ca/en/public-health/services/diseases/monkeypox.html.
Dashraath P, Nielsen-Saines K, Mattar C, Musso D, Tambyah P, Baud D. Guidelines for pregnant individuals with monkeypox virus exposure. Lancet. 2022;400(10345):21-22.
World Health Organization (WHO): Available at https://www.who.int/emergencies/situations/monkeypox-outbreak-2022.
Petersen E, Kantele A, Koopmans M, et al. Human Monkeypox: Epidemiologic and Clinical Characteristics, Diagnosis, and Prevention. Infect Dis Clin North Am. 2019;33(4):1027-1043.
US. Centers for Disease Control and Prevention (CDC): Available at https://www.cdc.gov.
Author
Cheryl Patterson RNC-TNP, BSN, Nurse Editor Adult Telehealth Triage Guidelines, STCC
Co-Authors
Jeanine Feirer, RN, MSN, Nurse Editor Adult Telehealth Triage, Guidelines, STCC
David Thompson MD, Senior Medical Editor, Adult Telehealth Triage Guidelines, STCC