About the Nurse Triage Benchmarking Survey
In May 2023, Schmitt-Thompson Clinical Content (STCC) requested feedback from nurses who work in a telehealth triage environment, whether a call center or provider office/clinic, about the services they provide and operational metrics from their contact center. We received 346 responses from nurses and nurse managers across the U.S. and Canada. As best we can calculate (due to duplicate responses from some organizations and other respondents who did not provide an email address), the results represent approximately 150+ different organizations. Many of the questions are intentionally the same as our 2017 and 2020 benchmarking studies allowing for trending comparisons.
2023 Nurse Triage Trends
In general, there haven’t been substantial changes to the services provided or operations of nurse telehealth triage call centers (e.g., same type of services provided, call length, and calls per hour). A couple metrics/topics where there were some significant changes, though, are identified below:
1. Increase in average call time compared to three years ago (Q7).
2. Increase in access to the patient’s electronic medical record during a triage encounter (Q13).
3. Increase in call centers who take calls for medical specialties (Q17).
4. Decrease in call centers who record their triage encounters (Q28).
5. Decrease in the number of call centers who charge for nurse advice services (Q34).
Question 1: Which of the following responses best describes the population managed by your call center?
Seventy percent (70%) of respondents manage both adult and pediatric populations. Sixteen percent manage adult only and 15% manage pediatric populations only.
Question 2: If your call center manages both adult and pediatric calls, approximately what percentage of callers are adult (age 18 years or older)?
Of the 70% who manage both adult and pediatric populations, 68% of the callers are age 18 or older and have adult symptoms (versus an adult calling on behalf of a child). One might surmise that nurse triage is mostly a service for adults based on the survey data, but it could also be reflective of the organizations who completed the survey.
Question 3: What type of calls are managed by your call center? (Check all that apply.)
“Types of calls managed by a call center” is a good metric to be knowledgeable about, but it may not indicate a trend based on the types of call centers who responded to this survey. For example, calls from insurance plan members appears to be declining, but is that truly the case or is it because insurance plans have their own call centers and members are calling there instead of the hospital/health system organizations surveyed for this study? Two categories of “types of calls” were added to the 2023 survey; nurse triage support for specialty clinics during daytime hours and during after-hours.
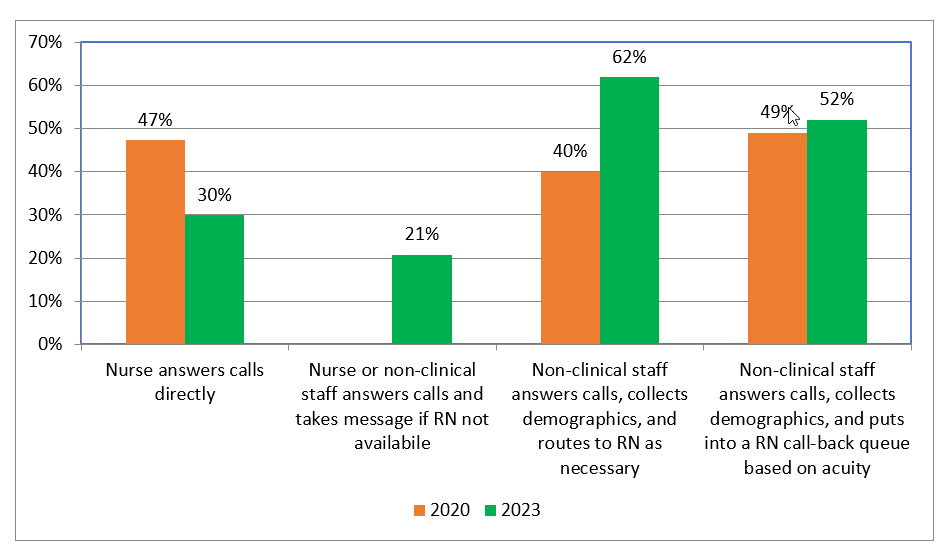
Question 4: What call intake strategy do you deploy in your call center? (Check all that apply.)
Even though two data points don’t necessarily make a trend (this question was not asked in 2017), it appears that there are fewer call centers utilizing nurses to answer calls directly. Instead, call centers are fronting the incoming calls with non-clinical staff. Some call centers may employ several of these options, causing some overlap in response percentages.
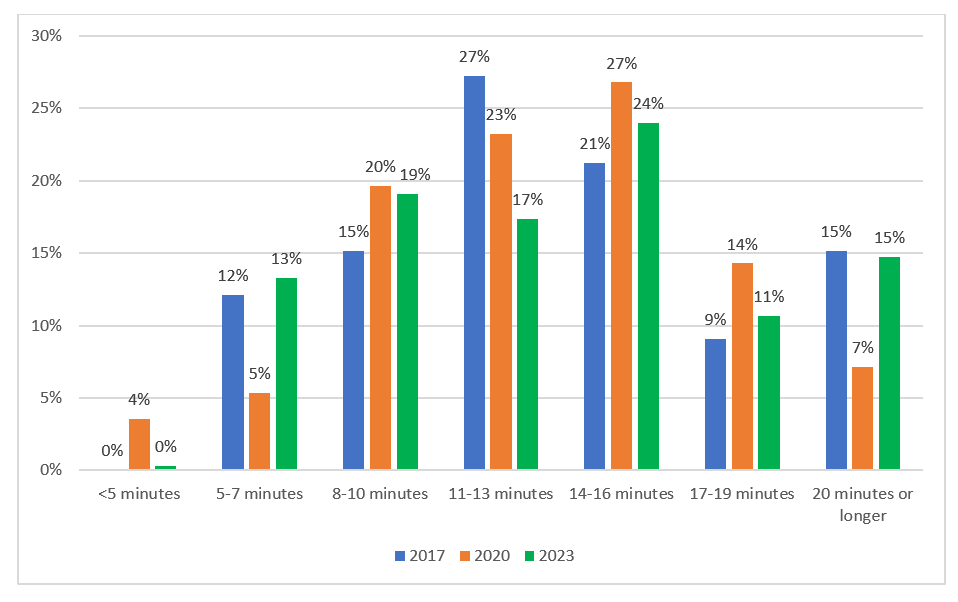
Question 5: What is the average triage call time (the time it takes to complete a call including documentation and after-call work)?
Over 40% of the respondents indicated their average call length was between 11 and 16 minutes, down a little bit from 50% in 2020. In 2023, there was an increase in the 20 minutes or longer call length category compared to 2020; 15% versus 7%. However, the same percentage of respondents in 2017 (15%) indicated their average call length was 20 minutes or longer. This might have something to do with the volume of calls received in 2020 related to COVID. If the majority of calls were COVID-related, nurses may have gotten adept at handling them and, therefore, there weren’t that many longer length calls.
Question 6: What type of additional after-call activities are included in your average triage call time? (Check all that apply)
The responses here clearly indicate that there is a lot more involved with a telehealth triage encounter besides just talking to the caller.
“Other” responses included:
· Routing of triage notes is automatic when verbal consent is given by caller.
· Any surgical patient that was not contacted during the day comes to us so we can give them their preoperative instructions.
· 911 or request welfare check.
· Calling ED to give report.
· Calling pharmacies. Our nurses document our ROI/productivity. They are internally documenting the patient’s disposition/referral to aid in a calculating a possible nurse triage service billable encounter.
· Calling pharmacy if needed. Sending refill requests to PCP with information needed for appropriate refills.
· Calling the receiving Emergency Room to give report.
· Care coordination with home care companies, social workers, etc.
· Charting. (5 responses)
· Completing paperwork, contacting specialties to expedite appointments, contacting pharmacies, insurance providers, DME providers, home health agencies, providing education.
· Contacting the on-call provider.
· Documenting my notes, updating a spreadsheet.
· Documenting notes from the interaction and advice given and sending to office.
· Documenting reason for call and outcome. Sending message or second-level triage to provider. Transferring to scheduling for appointments.
· Entering referrals, faxing documentation, sending follow-up MyChart message reiterating the information in writing for patients.
· Entering referrals, communicating with referral department, contacting specialists, contacting DME companies, home care, faxing prescriptions, referrals, plans of care, etc.
· Faxing records to specialists, employers; calling specialists, care managers or pharmacies regarding patient issue.
· Faxing what was requested. Mailing results, etc. Printing out test results to be mailed. Triage phone calls are usually lengthy and sometimes the other office needs to be called.
· Mandated reporting.
· Medication refills for virtual provider.
· Notify medical provider by sending them triage encounter as FYI if needed.
· Ordering all testing/imaging needed.
· Our triage team supports the practices with prescription refills, prior authorizations and smart set order entry based on quality metrics.
· Paging.
· Paging providers for second level triage if appropriate.
· Pending prescriptions for doctors, placing orders for labs and imaging, placing referrals.
· Reaching the on-call provider.
· Routing emergent/urgent messages to the offices with details of interaction.
· Scheduling is now more difficult and time consuming.
· Second level triage with midwives and ED physicians when appropriate.
· Sending info on MyChart as needed, collecting blood sugar logs.
· Sending notification of appointment made or disposition of patient on clinic's group chat.
· Separately tracking every call made and received for manager.
· Setting up My Connect, updating pharmacy, putting patient on waitlists, scheduling appointment with PCP if they are calling for a specialty and the appointment is too far out.
· Transferring caller to telehealth provider if necessary. Paging providers and sending messages for post op patients.
· Transferring registrant to EC Telemedicine Physician (EC Transfer); transferring to surgery provider (ASC Process); sending secure chat for surgery provider.
· We do nurse visits, fill in for the MA’s when they call in sick and room patients, handle walk-in patients and do prior authorizations and hospital follow-up calls during our day as well.
· We notify the office when patients decline ED visit, etc.
Question 7: How would you compare your average triage call time today to your average call time three years ago?
Forty-one percent of the 2023 respondents indicated their call times have significantly increased over the past three years; compared to only 29% who believe this was the case three years ago. As noted by some of the other responses to questions in this survey, it’s clear that the triage nurses are handling more responsibilities with their telehealth triage encounters leading to longer call times.
Question 8: If there has been an increase or decrease in the call time, what do you think are the main contributing factors? (Check all that apply.)
Question 9: How many calls does a nurse at your call center take, on average, per hour?
Even though the ratio has changed slightly over the past six years, in all three survey results, the majority of calls per hour fall into the 3 or 4 calls per hour category; 66% in 2017, 56% in 2020 and 46% in 2023. In contrast to the dip in the percentage of calls that fall into the “3” or “4” category in 2023, there was a higher percentage of respondents who indicated their nurses take 5 or 6 calls per hour.
Question 10: Does your call center offer or use second level triage (higher level triage or consultation by MD/PA or ARNP)?
The 2023 call center responses are almost evenly split between offering second level triage and not offering it; 49% and 51% respectively. And, there isn’t any trend for this question over the past six years. In 2017, 40% were not providing second level triage and 60% were providing it. In 2020, results indicate almost a complete reversal with 65% not providing second level triage and 35% providing second level triage.
Question 11: If yes, how do you manage second level triage?
A fourth response category of “triage nurse messaging/chatting with the provider and the provider calling the patient back” was added as an option in the 2023 survey making it difficult to see any trending. Of note, however, is that a higher percentage of respondents indicated that there is more true consultation with the provider versus a hand-off to the provider.
Question 12: If yes, what percentage of all call center triage calls use second level triage?
For those call centers that indicated they provide 2nd level triage, 48% use 2nd level triage in up to 20% of their triage encounters. Another 28% use 2nd level triage 20-50% of the time. Most call center respondents indicated they have a specific method to prioritize triage calls in their call center (71%) and of that 71% that prioritize calls, 43% indicated their current method could use improvement. There were a lot of comments to the open-ended question about describing the method to prioritize calls. The majority of the time there is a “red flag” or “hot calls” list that staff refer to for acuity of symptoms.
Question 13: Does the triage nurse at your call center have access to the patient's electronic medical record at the time of the call?
Research indicates it is overwhelmingly the norm in 2023 for the triage nurse to have access to a patient’s electronic medical record.
Question 14: Does your call center take calls for any medical specialty services/practices?
In the 2017 survey, only a little over one-quarter of respondents stated their call center took calls for medical specialty services or practices compared to almost 50% in 2023. It appears that these specialty groups are seeing the value of having a general call center take their nurse telehealth triage calls.
A follow-up question (question 15) was asked about the specialty services/practices that require a second level triage or consultation: For the 142 respondents who answered this question, the top medical specialty services that receive support from the telehealth triage nurses in the call center are: cardiology, OB/GYN/Women’s Services, endocrinology, orthopedics, gastroenterology, urology, general surgery, oncology and ophthalmology.
Question 15: Does your call center take calls/serve as an access point for telemedicine providers who provide virtual patient visits?
Almost half of the respondents (47%) indicated their call center serves as an access point for telemedicine providers who provide virtual patient visits. This is down slightly from the 2020 study (54%), which may have been impacted by COVID, but still almost double since 2017.
Question 16: If YES, can your nurses transfer a caller directly to a telemedicine provider or schedule an urgent telemedicine appointment?
In the 2020 survey, it was evenly split, 50/50, if call center nurses could transfer a call directly to a telemedicine provider or schedule an urgent telemedicine appointment. In 2023, fewer call center respondents (37%) indicated they could transfer or schedule an urgent telemedicine appointment. Either organizations have their own specific telemedicine scheduling departments in 2023 or the need for urgent telemedicine appointments have gone down and health systems/providers are not offering them as frequently or conveniently any longer.
Question 17: Do your nurses call in or electronically send prescription orders per approved standing orders/protocols for certain conditions?
Question 18: How does your call center handle requests for urgent prescription renewals after-hours? (Check all that apply).
Question 19: Do you have staff nurses who work remotely?
With 2020 being an anomaly due to the COVID pandemic, it appears that it has consistently been a 70/30% split between call centers who have nurses who work remotely and those that don’t.
Question 20: If YES, what percentage of your nursing staff is set up to work remotely?
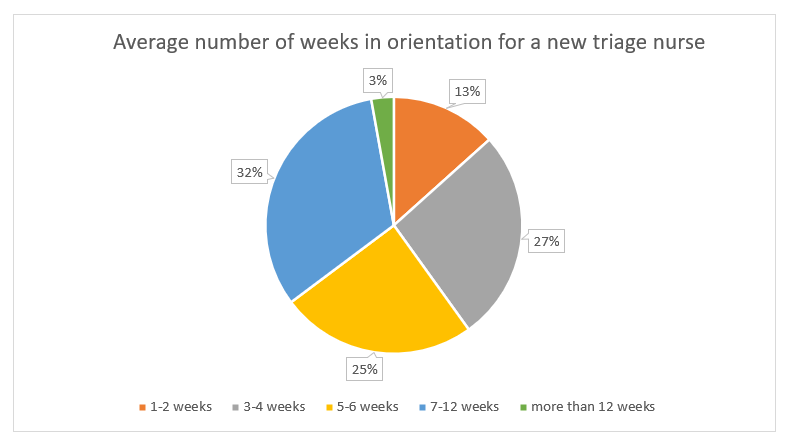
Question 21: How many weeks, on average, is a new triage nurse at your call center in orientation?
Question 22: How many years of nursing experience are required for employment as a triage nurse?
Question 23: Does your call center record triage calls?
An interesting trend over the past six years is that the number of call centers who record their triage calls has decreased substantially.
Question 24: If your call center records triage calls, how often are recorded calls reviewed for each RN, once orientation is completed?
Question 25: How does your call center measure patient/caller satisfaction? (Check all that apply.)
This question is difficult to evaluate regarding any trends since additional categories were added in 2023. However, it’s interesting to note that 57% of 2023 respondents (184 respondents) indicated no specific measurement of call center interaction satisfaction.
Question 26: Does your call center accept videos or photos sent from callers as part of the triage workflow?
In 2023, there appears to be almost an even 50/50 split between call centers that accept videos or photos as part of the triage workflow compared to previous years’ results.
Question 27: Do your triage nurses send any information to callers after a telephone interaction via email, text message or patient portal?
There was a slight uptick, from 2020 to 2023, in respondents who send information to their callers after a telephone interaction. Most of the time the “sending” is done via the patient’s portal rather than direct send; most likely this is due to privacy concerns with email or text.
Question 28: Do the nurses at your call center use online nurse chat with callers/patients?
There was a slight uptick in respondents who indicated the nurses use online nurse chat with callers over the past six years. However, based on the comments, it appears that “chat” was interpreted to mean via patient portal and not for nurse triage/advice services specifically.
Question 29: Does your call center charge for nurse advice services?
The majority of call centers, at 86% of 331 respondents, do not charge for nurse advice services. A trend that has continued for the past six years.
Question 30: If your call center charges for nurse advice services, what range does your fee fall into?
This question was not asked in the prior two surveys so there are no points of comparison. Note: the above percentages are based on only 33 responses.
Additional comments
· Annual increase is based on the Consumer Price Index.
· Around $37 for daytime and $43 for after-hours and specialty were the last numbers we derived. But we do not currently charge.
· Charge for external client triage business and for the past 2 years for daytime triage for primary care services. We do not charge for internal organization after-hours calls.
· Charges to doctors but I do not know the fee.
· Depends if it is an internal practice or not. Flat yearly fee for other types of calls; insurance line and college student health center.
· Depending on the subscriber and if they are a member of our organization or not.
· Flat fee for physicians and clinic. Patient does not pay.
· Our call charges are subsidized by our PCP physician network as part of the physician's benefit package (the PCP pays half and the network pays half). Our per call charge as described to the physicians is $10.81/call (without subsidy). We do provider services to 16 physicians not in our physician network, those calls are charged at $18.00 per call. The service to make next day appointments for physicians is optional and is charged to them at $5.00 per appointment in addition to the base call charge.
· Our calls are billed to the hospitals depending on the patient’s zip code.
· Outside community clinics only.
· Overnight ONLY charge to the department; not the patient.
· The physician practices that we are contracted with are charged $10 per call.
· The practice is charged a monthly maintenance fee of $135.
· There is a disclaimer that patients can be charged but so far, no mention.
· This is charged to companies that we contract with to provide services; not to callers/patients.
· We charge $12 for a plain triage call and $15 for a call with a script called in by RN. This price has not been updated in over 12 years.
· We only charge for services if the office is external. We do not charge for nurse triage services to practices that are part of our hospital system.
· We only charge the practices that we have contracted with to take their after-hours triage calls. They then receive a copy of our triage note. We have the ability to page their on-call provider and are sent monthly reports.
· We use a charge back model that is aligned with the charge back model for that practice.
Question 31: If YES, does that charge cover the actual cost (e.g., salary, benefits, overhead) of the call?
Of the 51 individuals who responded to the question, only 17%, or 15 respondents, indicated the charges cover the actual costs of the triage encounter. Interesting to note that three years ago 34% of the respondents to this question (29) indicated their charge covered the actual cost of the call. As we know, the cost of everything has gone up in three years, but not necessarily a corresponding charge for triage calls.
Question 32: What other services does your call center offer? (Check all that apply.)
Schmitt-Thompson Clinical Content thanks you for your continued support of our research endeavors and making the world of telehealth triage safer. For more information, please reach out to info@stcc-triage.com.